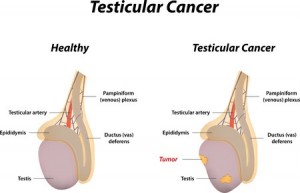
Testicular cancer occurs in the testicles (testes), which are located inside the scrotum, a loose bag of skin underneath the penis. The testicles produce male sex hormones and sperm for reproduction.
Testicular cancer is highly treatable, even when cancer has spread beyond the testicle. Depending on the type and stage of testicular cancer, you may receive one of several treatments, or a combination. Regular testicular self-examinations can help identify growths early, when the chance for successful treatment of testicular cancer is highest.
Symptoms
Signs and symptoms of testicular cancer include:
• A lump or enlargement in either testicle
• A feeling of heaviness in the scrotum
• A dull ache in the abdomen or groin
• A sudden collection of fluid in the scrotum
• Pain or discomfort in a testicle or the scrotum
• Enlargement or tenderness of the breasts
• Back pain
Cancer usually affects only one testicle.
Causes
It’s not clear what causes testicular cancer in most cases.
Doctors know that testicular cancer occurs when healthy cells in a testicle become altered. Healthy cells grow and divide in an orderly way to keep your body functioning normally. But sometimes some cells develop abnormalities, causing this growth to get out of control — these cancer cells continue dividing even when new cells aren’t needed. The accumulating cells form a mass in the testicle.
Nearly all testicular cancers begin in the germ cells — the cells in the testicles that produce immature sperm. What causes germ cells to become abnormal and develop into cancer isn’t known.
Risk factors
Factors that may increase your risk of testicular cancer include:
• An undescended testicle (cryptorchidism). The testes form in the abdominal area during fetal development and usually descend into the scrotum before birth. Men who have a testicle that never descended are at greater risk of testicular cancer in either testicle than are men whose testicles descended normally. The risk remains elevated even if the testicle has been surgically relocated to the scrotum.
Still, the majority of men who develop testicular cancer don’t have a history of undescended testicles.
• Abnormal testicle development. Conditions that cause testicles to develop abnormally, such as Klinefelter’s syndrome, may increase your risk of testicular cancer.
• Family history. If family members have had testicular cancer, you may have an increased risk.
• Age. Testicular cancer affects teens and younger men, particularly those between ages 15 and 35. However, it can occur at any age.
• Race. Testicular cancer is more common in white men than in black men.
•
Tests and diagnosis
In some cases men discover testicular cancer themselves, either unintentionally or while doing a testicular self-examination to check for lumps. In other cases, your doctor may detect a lump during a routine physical exam.
To determine whether a lump is testicular cancer, your doctor may recommend:
• Ultrasound. A testicular ultrasound test uses sound waves to create an image of the scrotum and testicles. During an ultrasound you lie on your back with your legs spread. Your doctor then applies a clear gel to your scrotum. A hand-held probe is moved over your scrotum to make the ultrasound image.
• Blood tests. Your doctor may order tests to determine the levels of tumor markers in your blood. Tumor markers are substances that occur normally in your blood, but the levels of these substances may be elevated in certain situations, including testicular cancer. A high level of a tumor marker in your blood doesn’t mean you have cancer, but it may help your doctor in determining your diagnosis.
• Surgery to remove a testicle (radical inguinal orchiectomy). If it’s determined that the lump on your testicle may be cancerous, surgery to remove the testicle may be recommended. Your removed testicle will be analyzed to determine if the lump is cancerous and, if so, what type of cancer.
Determining the type of cancer
Your extracted testicle will be analyzed to determine the type of testicular cancer. The type of testicular cancer you have determines your treatment and your prognosis. In general, there are two types of testicular cancer:
• Seminoma. Seminoma tumors occur in all age groups, but if an older man develops testicular cancer, it is more likely to be seminoma. Seminomas, in general, aren’t as aggressive as nonseminomas.
• Nonseminoma. Nonseminoma tumors tend to develop earlier in life and grow and spread rapidly. Several different types of nonseminoma tumors exist, including choriocarcinoma, embryonal carcinoma, teratoma and yolk sac tumor.
Staging the cancer
Once your doctor confirms your diagnosis, the next step is to determine the extent (stage) of the cancer. To determine whether cancer has spread outside of your testicle, you may undergo:
• Computerized tomography (CT) scan. CT scans take a series of X-ray images of your abdomen, chest and pelvis. Your doctor uses CT scans to look for signs that cancer has spread.
• Blood tests. Blood tests to look for elevated tumor markers can help your doctor understand whether cancer likely remains in your body after your testicle is removed.
After these tests, your testicular cancer is assigned a stage. The stage helps determine what treatments are best for you. The stages of testicular cancer are:
• Stage I. Cancer is limited to the testicle.
• Stage II. Cancer has spread to the lymph nodes in the abdomen.
• Stage III. Cancer has spread to other parts of the body. Testicular cancer most commonly spreads to the lungs and liver.
Treatments and drugs
The options for treating your testicular cancer depend on several factors, including the type and stage of cancer, your overall health, and your own preferences.
Surgery
Operations used to treat testicular cancer include:
• Surgery to remove your testicle (radical inguinal orchiectomy) is the primary treatment for nearly all stages and types of testicular cancer. To remove your testicle, your surgeon makes an incision in your groin and extracts the entire testicle through the opening. A prosthetic, saline-filled testicle can be inserted if you choose.
• Surgery to remove nearby lymph nodes (retroperitoneal lymph node dissection) is performed through an incision in your abdomen. Your surgeon takes care to avoid damaging nerves surrounding the lymph nodes, but in some cases harm to the nerves may be unavoidable. Damaged nerves can cause difficulty with ejaculation, but won’t prevent you from having an erection.
In cases of early-stage testicular cancer, surgery may be the only treatment needed.
If surgery is your only treatment for testicular cancer, your doctor will recommend a schedule of follow-up appointments. At these appointments — typically every few months for the first few years and then less frequently after that — you’ll undergo blood tests, CT scans and other procedures to check for signs that your cancer has returned.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays, to kill cancer cells. During radiation therapy, you’re positioned on a table and a large machine moves around you, aiming the energy beams at precise points on your body.
Radiation therapy is a treatment option that’s sometimes used in people who have the seminoma type of testicular cancer. Radiation therapy may be recommended after surgery to remove your testicle.
Side effects may include fatigue, as well as skin redness and irritation in your abdominal and groin areas. Radiation therapy is also likely to cause infertility. Talk to your doctor about your options for preserving your sperm before beginning radiation therapy.
Chemotherapy
Chemotherapy treatment uses drugs to kill cancer cells. Chemotherapy drugs travel throughout your body to kill cancer cells that may have migrated from the original tumor.
Chemotherapy may be your only treatment, or it may be recommended before or after lymph node removal surgery.
Side effects of chemotherapy depend on the drugs being used. Ask your doctor what to expect. Common side effects include fatigue, nausea, hair loss and an increased risk of infection. There are medications and treatments available that reduce some of the side effects of chemotherapy.
Chemotherapy is also likely to cause infertility, which can be permanent. Talk to your doctor about your options for preserving your sperm before beginning chemotherapy.
Prevention
There’s no way to prevent testicular cancer.
Some doctors recommend regular testicle self-examinations to identify testicular cancer at its earliest stage. But not all doctors agree. Discuss testicular self-examination with your doctor if you’re unsure about whether it’s right for you.
If you choose to do a testicular self-examination, a good time to examine your testicles is after a warm bath or shower. The heat from the water relaxes your scrotum, making it easier for you to find anything unusual.
To do this examination, follow these steps:
• Stand in front of a mirror. Look for any swelling on the skin of the scrotum.
• Examine each testicle with both hands. Place the index and middle fingers under the testicle while placing your thumbs on the top.
• Gently roll the testicle between the thumbs and the fingers. Remember that the testicles are usually smooth, oval shaped and somewhat firm. It’s normal for one testicle to be slightly larger than the other. Also, the cord leading upward from the top of the testicle (epididymis) is a normal part of the scrotum. By regularly performing this exam, you can become more familiar with your testicles and aware of any changes that might be of concern.